Vomiting Blood (Hematemesis): Causes, Symptoms & Treatment
- September 18, 2025
- City Hospital
Understanding Vomiting Blood
Vomiting blood(throwing up blood), medically known as hematemesis, is a frightening symptom that signals internal bleeding. Whether you’re vomiting blood along with stomach contents or blood by itself, it’s essential to understand what’s going on in your body. Hematemesis may present itself as fresh, bright red blood or darker, coagulated blood, often resembling coffee grounds.
This condition typically points to bleeding in the upper digestive tract — the esophagus, stomach, or duodenum (the first part of your small intestine). Since this can be a sign of a serious condition, immediate medical attention is crucial.
Is Vomiting Blood a Serious Condition?
Vomiting blood can be alarming, but the severity depends on the underlying cause. While some causes are relatively benign, others are life-threatening. Healthcare providers treat all cases of hematemesis as emergencies until they can determine the cause. Therefore, if you notice any signs of vomiting blood, it’s vital to seek medical care immediately.
Is a Small Amount of Blood in Vomit Normal?
Even a small amount of blood in vomit is not considered normal. While minor bleeding might occur from the physical trauma of vomiting, other causes might point to an underlying medical issue. Never ignore the presence of blood in your vomit — it’s important to consult a healthcare provider regardless of the amount.
Can Vomiting Blood Lead to Death?
While vomiting itself is unlikely to be fatal, the significant blood loss associated with hematemesis can lead to hypovolemic shock — a life-threatening condition caused by severe blood loss. Shock can cause organ failure and, if left untreated, even death. The key to surviving hematemesis lies in early detection and prompt treatment.
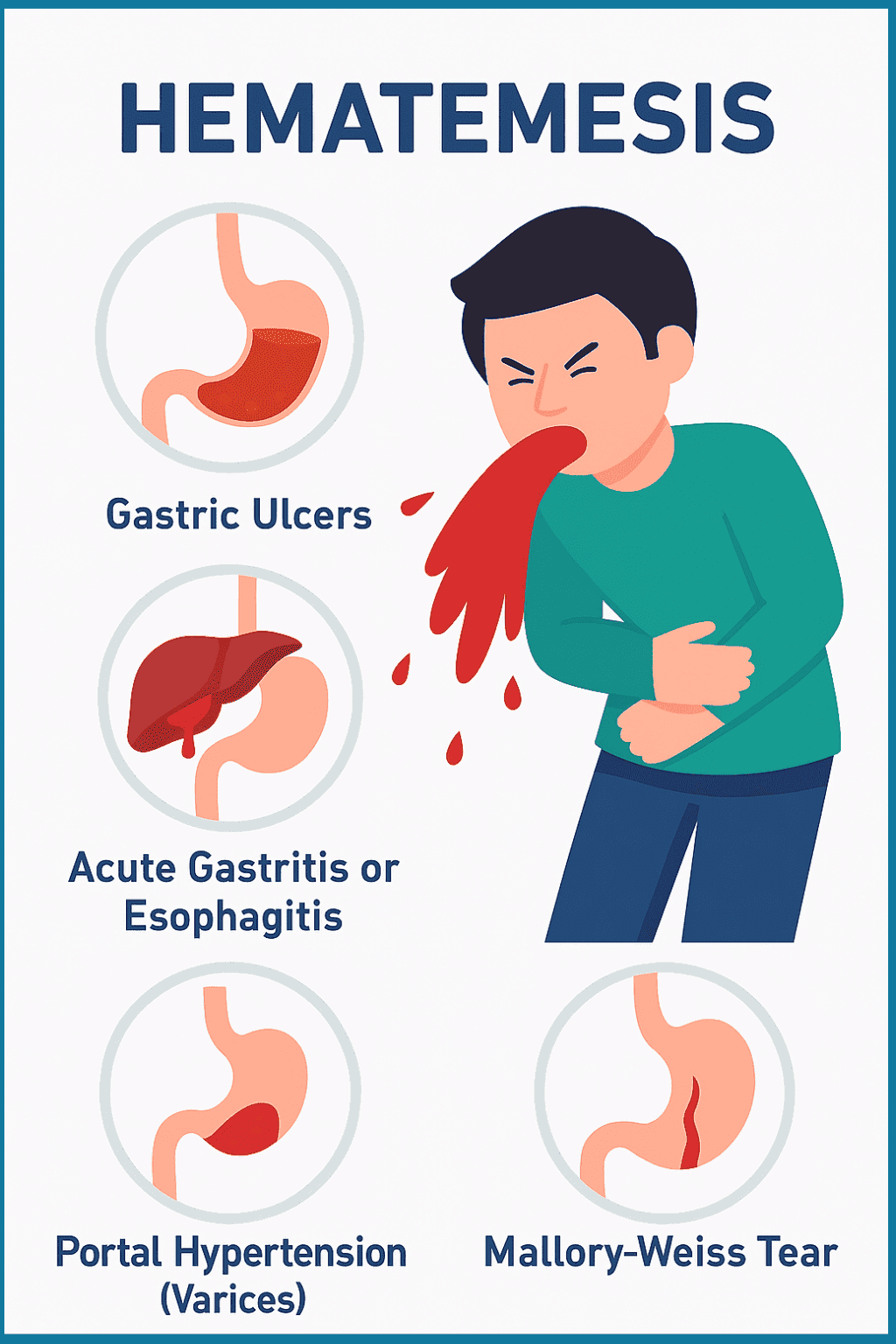
What Causes Hematemesis?
Vomiting blood can result from various conditions affecting the upper digestive system. The most common causes include:
Gastric Ulcers (Peptic Ulcers)
Peptic ulcers are open sores that develop on the stomach lining or the duodenum. These ulcers can erode blood vessels, causing bleeding, which may result in vomiting blood. Common causes of peptic ulcers include bacterial infections (like Helicobacter pylori) or excessive use of nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin.
Acute Gastritis or Esophagitis
Inflammation of the stomach lining (gastritis) or the esophagus (esophagitis) can lead to the rupture of small blood vessels beneath the lining, resulting in blood being vomited. Conditions such as severe acid reflux, excessive alcohol consumption, and the prolonged use of NSAIDs can cause these inflammations.
Portal Hypertension (Varices)
Portal hypertension, often due to liver cirrhosis, increases the pressure in the veins surrounding the esophagus and stomach. This can lead to the formation of varices (enlarged veins), which are fragile and prone to rupture, causing significant bleeding. Vomiting blood from varices is a medical emergency.
Mallory-Weiss Tear
A Mallory-Weiss tear is a tear in the esophagus, typically caused by violent or forceful vomiting. This condition is often associated with heavy drinking or eating disorders, and can result in significant blood loss.
Tumors or Cancers
Tumors, whether benign or malignant, in the esophagus, stomach, or pancreas can cause bleeding. Cancerous tumors, in particular, may cause slow or intermittent bleeding, leading to vomiting blood.
Angiodysplasias
These are abnormal blood vessels in the stomach and intestines, which can rupture and cause bleeding. They are often seen in older adults and may cause recurrent episodes of hematemesis.
Trauma or Injury
Physical trauma to the stomach or esophagus, such as blunt force or injury during medical procedures, can result in bleeding and vomiting blood. In some cases, even minor injuries can lead to significant internal bleeding.
Chronic Pancreatitis
Long-term inflammation of the pancreas (chronic pancreatitis) can damage nearby blood vessels, leading to bleeding that may flow into the duodenum, causing vomiting of blood.
What Are the Symptoms of Hematemesis?
Vomiting blood is usually accompanied by other symptoms, which can help healthcare providers determine the underlying cause:
Bright Red Blood: Indicates fresh bleeding from the upper digestive tract.
Coffee Ground-Like Vomit: Indicates older, digested blood, often from the stomach or duodenum.
Dizziness or Fainting: A sign of blood loss and potential hypovolemic shock.
Pain in the Abdomen: Could be due to an ulcer or inflammation.
Rapid Heartbeat and Shortness of Breath: Signs of severe blood loss.
Paleness and Weakness: Often associated with anemia caused by blood loss.
If you experience any of these symptoms along with vomiting blood, seek immediate medical help.
How Is Hematemesis Diagnosed?
When you present with vomiting blood, healthcare providers will begin by taking a thorough medical history and performing a physical examination. Key steps in diagnosing hematemesis include:
Endoscopy
An upper endoscopy is often the first diagnostic tool used. During this procedure, a flexible tube with a camera is inserted down the throat to view the esophagus, stomach, and duodenum. This allows the doctor to locate the source of bleeding, and sometimes stop the bleeding during the procedure.
Blood Tests
Blood tests help assess the extent of blood loss and determine your overall health. Tests for liver function, anemia, and clotting ability may also be performed.
Imaging Studies
In certain cases, imaging tests like CT scans or ultrasounds may be used to evaluate other organs, such as the liver or pancreas, to rule out other causes of bleeding.
Treatment for Hematemesis
The treatment for vomiting blood depends on the underlying cause and the severity of the bleeding. Common treatment steps include:
Immediate Care
If you’re experiencing severe blood loss, emergency care is needed to stabilize your condition. Intravenous fluids, blood transfusions, and oxygen support are often administered to prevent shock.
Medications
Once the immediate threat is controlled, medications may be prescribed to manage the underlying cause. For example, proton pump inhibitors (PPIs) may be used to reduce stomach acid and help ulcers heal. Vasopressors or clotting agents may be used if the bleeding is from varices.
Endoscopic Procedures
In many cases, endoscopy can be used to treat bleeding. If the source of the bleeding is found, the doctor may use special tools to cauterize the wound, apply a bandage to varices, or inject medications to stop the bleeding.
Surgical Intervention
If endoscopic treatment isn’t sufficient or if the bleeding is severe, surgery may be required to repair ulcers, stop bleeding from varices, or remove tumors.
Note: Always Consult
Preventing Hematemesis
While not all cases of hematemesis are preventable, the following steps can help reduce your risk:
Manage Acid Reflux and Gastritis: Avoid triggers like spicy foods, alcohol, and NSAIDs. Taking medications as prescribed can help manage these conditions.
Limit Alcohol Consumption: Chronic alcohol use is a significant risk factor for bleeding ulcers and varices.
Quit Smoking: Smoking can aggravate ulcers and increase the risk of bleeding.
Get Regular Check-ups: If you have conditions like cirrhosis, ulcers, or a history of digestive bleeding, regular check-ups with your doctor are essential.
Take Action Now – Consult Our Specialist for Hematemesis Treatment
Vomiting blood is never a symptom to ignore. Whether it appears as bright red blood or dark, coffee ground-like material, hematemesis is often a sign of serious internal bleeding that needs immediate medical evaluation.
Conditions such as stomach ulcers, esophageal tears, variceal bleeding, or even gastrointestinal surgery cancers could be behind this alarming symptom — and the longer you wait, the more serious it can become.
Here’s how we can help you:
Immediate evaluation and stabilization in urgent cases
Consultation with expert gastroenterologists
Safe and minimally invasive procedures to control bleeding
Customized treatment plans based on your health history
Ongoing support and lifestyle guidance for prevention
FAQs (Frequently Asked Questions)
If you vomit blood, seek emergency medical care immediately. The cause of the bleeding must be identified and treated promptly.
Yes, vomiting blood is often a sign of a serious condition such as ulcers, cancer, or liver disease. It requires immediate medical evaluation.
Recovery time depends on the cause of the bleeding and the treatment required. Some cases may require weeks of recovery, while others may need longer-term management.
While less common in children, hematemesis can occur due to conditions such as accidental ingestion of toxins, infections, or rare digestive disorders. Immediate evaluation by a healthcare provider is necessary.
Search Keywords